“Green” Offices are Healthier: New Analysis
Author: Todd L Sack MD FACP 
We know that hospitals create a lot of hazardous pollution: air pollution, chemical waste, bio-hazards, dirty water, and greenhouse gases. A 2016 study by Matthew Eckelman and Jodi Sherman from Northeastern and Yale and Northeastern universities, respectively, looked beyond the role of hospitals to find that the entire United States healthcare system is far worse.1 Healthcare is responsible for 10% of America’s smog-producing chemicals and the same share of greenhouse gases.1 And healthcare’s energy consumption and emissions grew by 28% over ten years at a time when total US energy use diminished slightly.1
When the authors matched this energy use with estimates of the amounts of air pollution created and the health impacts, they found that healthcare’s pollution is responsible for a staggering 405,000 years of life lost annually in the US! Eckelman and Sherman concluded that, “Health care pollution itself is a patient safety issue and pollution prevention ought to be included in ongoing efforts to improve health care safety and quality overall.”1
Hospitals are responsible for about a third of these emissions and perhaps 145,000 years of life lost in the US annually due to diseases attributed to air pollution. As bad as these numbers seem, hospitals around the world are learning to use energy and other resources more efficiently. Organizations such as Health Care Without Harm, founded in 1996, work with hospital systems in more than fifty countries.
I analyzed the Eckelman and Sherman data to draw attention to the health harms caused by outpatient care. There are thousands more clinics, offices, dental practices, surgical centers, rehabilitation centers, and laboratories than there are hospitals. A lot of care occurs in nursing homes, retirement communities, and private homes as well. Each of these contributes to pollution, greenhouse gases & illness. Each is an opportunity to improve and save money.
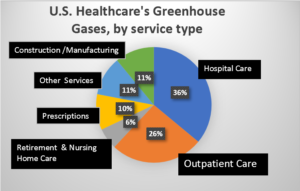 This pie chart shows each health care sector’s contribution to the industry’s total greenhouse gases. The results for other air pollutants are similar to these for greenhouse gases. The category “Outpatient Care” groups together the non-hospital services from medical doctors, dentists, home care, public health departments, and other professional services. Other terms in the chart are explained below.2
This pie chart shows each health care sector’s contribution to the industry’s total greenhouse gases. The results for other air pollutants are similar to these for greenhouse gases. The category “Outpatient Care” groups together the non-hospital services from medical doctors, dentists, home care, public health departments, and other professional services. Other terms in the chart are explained below.2
Outpatient healthcare is responsible for at least 26% of the industry’s harmful air pollution and greenhouse gases. This means that more than 105,000 years of life are lost in the US alone from the air pollution created by outpatient medicine. Not included here are the non-lethal sufferings of children with asthma attacks, people with cancers caused by air toxics from burning fossil fuels, and adult victims of heart attacks & respiratory illness. No one to date has calculated the additional costs of the health impacts and the environmental degradation resulting from water pollution, plastics use, and solid wastes from the healthcare industry.
In 2013, the US Institute of Medicine recommended that “the health sector should lead by example by greening itself and reducing its ecological footprint.”3 There are tremendous opportunities for healthcare offices to save money and to improve community health outcomes with environmentally sustainability. A five-office group in Pensacola, Florida committed itself to this several years ago. With no financial investments, they began saving energy and money in the first month. Over the first year, they lowered their electricity bill by 5.2%, saved $1500 per doctor, and reduced their greenhouse gas production by 85,600 pounds of CO2, which was the equivalent of not burning 4,349 gallons of gasoline.4 These results, if extended across the world’s hundreds of thousands of sites of outpatient care, would have a substantial impact upon community health. Even more powerful would be for health professionals to teach their patients some of these wise choices for using energy, water, chemical, plastics, transportation, and foods.
There are several free resources that health professionals can use to “go green”.5 The My Green Doctor service is the easiest to use. Accessed at https://mygreendoctor.org , this is the world’s most widely-used program for forging a “green” office. My Green Doctor is managed by health professionals, is evidence-based, and is comprehensive. The program adds only five minutes to each office or clinic planning meeting, and there is nothing for the office manager to study because each meeting’s five minutes of Green Team business is fully scripted in the “Meeting-by-Meeting Guide”.
Outpatient health care contributes to human suffering through the waste of energy and other forms of pollution. “Green” offices save money and are healthier. Register today at My Green Doctor and ask your colleagues to support making environmental sustainability a goal for your practice.
References & Methods
- Eckelman MJ, Sherman J (2016) “Environmental Impacts of the U.S. Health Care System and Effects on Public Health”. PLoSONE11 (6): e0157014. doi:10.1371/journal.pone.0157014
- The pie chart regroups the data from Eckelman & Sherman’s “Table 1. Absolute healthcare greenhouse gas emissions (MtCO2-e) by National Health Expenditure category and U.S. total for 2003–2013”.1 The categories originate from the National Health Expenditure Accounts database.6 The chart uses only the data from 2013 because the Table’s earlier data does not incorporate the lessened dangers of energy use that have resulted from America’s ongoing transition from coal to natural gas and to renewable energy. “Outpatient Care” does not include the care in hospital-owned clinics that often is billed as hospital services, but does includes the category “Public Health” because the latter are largely office-based services. “Construction/Manufacturing” includes the energy needed to build buildings and medical equipment. “Other Services” groups together energy use data for several sectors: “Durable Medical Equipment”, “Other Non-Durable Medical Products”, “Government Administration”, “Net Cost of Health Insurance”, and “Research”.
- Institute of Medicine Roundtable on Environmental Health Sciences and Medicine. Public Health Linkages with Sustainability Workshop Summary. Washington DC: National Academies Press; 2013.
- “Success Stories”, https://mygreendoctor.org/profiles/ . Accessed 29 November 2020.
- “Useful Websites”, https://mygreendoctor.org/resources/ . Accessed 29 November 2020.
- Centers for Medicare & Medicaid Services. National Health Expenditure Data. Available: http://www. cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/ NationalHealthExpendData/index.html. Accessed 29 November 2020.
About the Author:
 Todd L Sack MD, FACP is Editor of My Green Doctor, the world’s leading environmental sustainability program for outpatient healthcare offices, clinics, bureaus, and other facilities. Fourteen health professionals societies provide My Green Doctor to their members as a money-saving membership benefit. Your comments are welcome: [email protected] .
Todd L Sack MD, FACP is Editor of My Green Doctor, the world’s leading environmental sustainability program for outpatient healthcare offices, clinics, bureaus, and other facilities. Fourteen health professionals societies provide My Green Doctor to their members as a money-saving membership benefit. Your comments are welcome: [email protected] .

